How Can I Receive Insurance Coverage?
All major insurances have coverage policies for TMS outside Medicaid. Medicaid unfortunately does not cover TMS in the state of CO. Each insurer has specific criteria, so be sure to consult with your personal insurance company, though they generally share similar policies. For instance, TMS treatment for major depression often requires a patient to be unresponsive to (or not tolerate) previous medication from 2 different classes of antidepressants. Inspire TMS Denver works with all major insurance companies. We are experienced in navigating policy requirements and can assist you with understanding insurance criteria and the process of applying for coverage. We also provide an estimate of out of pocket costs not covered by your insurance (deductible, copay, or coinsurance) for TMS treatment.
Major insurers in CO and their coverage policies
To follow is a brief summary of major insurers in CO and their coverage policies. These are subject to change and based on our own research. Please consult your insurance to verify. For all insurers, these basic criteria are required:
- Patient is 18 years of age or older. TMS is now FDA approved to treat major depressive disorder in adolescents down to age 15, but most insurers do not have coverage policies for this age group yet.
- Patient has a current diagnosis of Major Depressive Disorder and the severity is at least moderate to severe based on a standardized rating scale (such as the PHQ-9).
- The current episode of depression must have some level of treatment resistance. This typically involves a range of antidepressant failure from as little as one up to as many as four failed medications. The medication trials must be of adequate duration and dose and have resulted in less than 50% improvement based on a standard rating scale. Medication intolerance can also count in place of lack of response.
- A documented previous course of failure to psychotherapy of sufficient time and frequency is also often required.
- Prior treatment response to TMS of at least 50% improvement in symptoms can alternatively be used to authorize repeat treatment. Maintenance treatment is NOT covered, but retreatment with sufficient time having passed since the last TMS therapy course is covered.
- If a patient is a candidate for ECT, but cannot pursue or declines ECT treatment for a valid concern (or has a history of intolerance/side effects to ECT), TMS will typically be covered.
- There are a few exclusion criteria to TMS - The patient cannot have ferromagnetic material near the brain/treatment site or medical devices in the neck or head that may respond to magnetic fields. The patient should also not have active psychosis (or a psychotic disorder diagnosis), current suicide intent or action, active abuse of alcohol or drugs, or be pregnant or nursing. The patient must also not have a seizure disorder or other condition that places them at high risk for seizure.
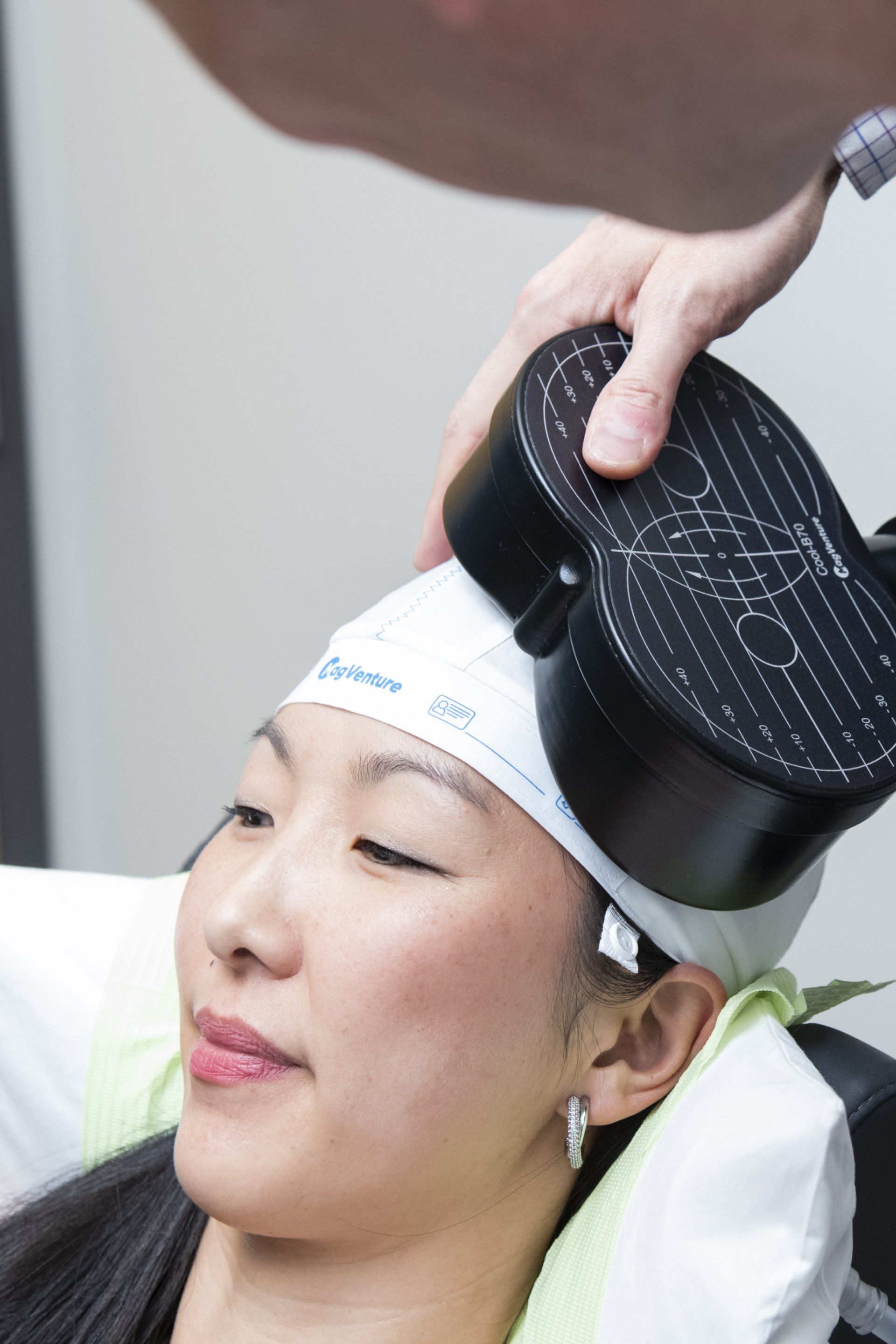
A covered course of TMS therapy typically involves 30 treatments daily M-F for 6 weeks with an additional 6 tapering treatments spread over 3 weeks. It must be prescribed and monitored by a Psychiatrist or similar provider with psychiatric medication prescribing privileges. Rating scales must be utilized during care.
Insurance coverage for TMS treatment in other Mental Health Disorders
Obsessive Compulsive Disorder has been shown to respond to TMS therapy and TMS was approved for augmentation OCD treatment by the FDA in 2018. Unfortunately, many insurance providers are slower to add newer therapies to their policies, but Cigna and some non-Anthem BCBS plans do have coverage policies supporting TMS for OCD. Other mental health disorders including PTSD and anxiety disorders have also demonstrated significant benefits from TMS but are not, as yet, approved by the FDA for TMS treatment and consequently are omitted from insurance coverage.
Inspire TMS Denver works closely with our insurance benefits and billing department to ensure patients are fully informed of any copay, coinsurance, and/or deductible that may be required for services. Inspire TMS Denver also establishes single case agreements for any clients with insurance that we are not paneled with currently.
How Much Does TMS Therapy Cost?
Sliding Scale Pricing (Applies to Self-Pay Patients Only)
Transcranial Magnetic Stimulation-TMS, was approved by the FDA for treating treatment resistant major depression in 2008. Currently, all insurance companies (outside CO Medicaid) now cover
TMS for treatment resistant major depression. Additional indications for TMS are growing and coverage likewise will continue to increase in the future. Some insurers also cover other treatment resistant conditions such as OCD (which now has FDA approval for TMS use as an augmentation treatment). TMS treatment costs can be quite affordable depending on insurance coverage, copays and coinsurance amounts for your plan, and any deductible met for the year. Treatment is sometimes fully covered by insurance or a small copay may be owed at each treatment. We provide free estimates for cost of care prior to treatment initiation.
Inspire TMS Denver also provides sliding scale self-pay rates for individuals that may pursue off-label treatment or not qualify for insurance coverage. We only provide TMS off-label when we feel there is sufficient evidence base and safety data. Rates as listed below:
| Gross Family Income | Accelerated TMS - 50 sessions in 1 week | Standard TMS Course (pre-paid option) | Standard TMS Course (pay as you go) | Maintenance TMS |
|---|---|---|---|---|
| >$300,000 | $12,000 | $10,500 | $11,950 | $200 |
| $250,000-$300,000 | $11,000 | $9,500 | $10,755 | $180 |
| $200,000-$250,000 | $10,000 | $8,500 | $9,560 | $160 |
| $150,000-$200,000 | $9,000 | $7,500 | $8,365 | $140 |
| $100,000-$150,000 | $8,000 | $6,500 | $7,170 | $120 |
| <$100,000 | $7,000 | $5,500 | $5,975 | $100 |
Pricing Breakdown
| Gross Family Income | Initial Mapping + Treatment | Regular Treatment | Remapping + Treatment | Eval | Follow Up |
|---|---|---|---|---|---|
| >$300,000 | $400 | $300 | $350 | $400 | $150 |
| $250,000-$300,000 | $360 | $270 | $315 | $360 | $135 |
| $200,000-$250,000 | $320 | $240 | $280 | $320 | $120 |
| $150,000-$200,000 | $280 | $210 | $245 | $280 | $105 |
| $100,000-$150,000 | $240 | $180 | $210 | $240 | $90 |
| <$100,000 | $200 | $150 | $175 | $200 | $75 |
We also provide initial phone TMS consultations FREE of charge, giving clients the peace of mind to explore TMS as a treatment option before deciding to establish care with a full evaluation and TMS therapy. No costs or obligations are involved for this and typically involves 10-15 minutes to discuss TMS treatment in brief and answer any questions. In addition, we do not charge any fees for add-on protocols, such as anxiety or PTSD protocols or iTBS treatment for depression. Please contact us here for a free phone consultation with Dr. Clinch.