LOCATION
340 East 1st Avenue, Suite 333 Broomfield, CO 80020
PHONE
720-446-8675
BUSINESS HOURS
- Mon - Fri
- -
- Sat - Sun
- Closed
Response Rates
10,000+ Treatments Completed
Is TMS Therapy Right For Me?
Take the short quiz below to see if you might be a good candidate for TMS. We've also answered all your key questions on how much TMS costs, conditions treated, who is eligible and much more!
Transcranial Magnetic Stimulation (TMS) Therapy is an excellent treatment option for depression and anxiety with extensive research supporting its results, but how can you know if it is the right treatment for you?
We all experience low mood or overwhelming stress at times. However, these feelings can persist and develop into mental health conditions, such as Major Depressive Disorder, Generalized Anxiety Disorder, or Panic Disorder. These can be recurrent or potentially long-term conditions that impact your day-to-day life. Symptoms can present with no obvious cause or be in reaction to stressful events in our lives.
Frontline treatments for depression and anxiety usually consist of antidepressants and counseling. For many, this can be an effective solution for recovery and relief from depression and anxiety. Unfortunately, this does not work for everyone. Some ⅓ of all individuals seeking treatment will experience treatment resistant depression or fail to respond to standard treatments.¹
Transcranial Magnetic Stimulation (TMS) is an alternative option for patients who do not find relief with medication or therapy, or who suffer from adverse side effects from antidepressants.
To decide if TMS is right for you, we recommending asking yourself the following 4 questions:
-
1. Do I have a mental health condition that TMS is indicated for?
TMS is FDA-approved for treating major depressive disorder (MDD) and obsessive-compulsive disorder (OCD). It can also be used off-label to treat other mental health conditions such as anxiety, panic, and post-traumatic stress disorder (PTSD). If you have been diagnosed with any of these conditions, TMS could be a good treatment option for you.
-
2. Have I tried other treatment options?
Since insurance typically doesn't cover TMS unless you have tried other treatment options such as medication, therapy, or a combination of both, TMS is generally considered a second-line option. Although each insurer’s criteria varies, we generally recommend trying at least 2 different medications from different classes (eg an SSRI - Lexapro, Celexa, Zoloft, Prozac, Paxil; SNRI - Pristiq, Effexor, Cymbaltal; NDRI - Wellbutrin; or some other class of antidepressant - TCA, Lithium, Remeron, Abilify). We also recommend trying counseling.
-
3. Do I have any contraindications for TMS?
While TMS is generally safe and very well tolerated, some conditions may prevent you from receiving treatment or insurance may not cover treatment due to insufficient evidence base for your particular condition. These include a history of seizures, metal implants or magnetically influenced devices in your head, diagnosis of Schizophrenia or Bipolar, current psychotic symptoms, or current substance abuse. Please know that some of these conditions may still be suitable for treatment, but will need to be pursued via self-pay as insurance unfortunately does not cover TMS for these diagnoses.
-
4. Are you able to commit to TMS?
TMS therapy is a considerable time commitment, consisting of 36 total treatments that take place over 9 weeks. The first 6 weeks you receive 5 treatments a week, Monday through Friday. The last 3 weeks you are on a taper schedule with 3 treatments one week, 2 treatments the next week, and one treatment on your final week. Each appointment in the office typically lasts about 30 minutes.
TMS was originally approved by the FDA and later adopted by health insurance companies for treatment-resistant depression and our results with TMS speak for themselves,
https://www.inspiretmsdenver.com/inspire-tms-clinic-results
We achieve excellent results for depression, anxiety, PTSD, and OCD, offering a medication-free treatment option with only limited and localized minor side effects at most. Given the not uncommon side effects, potential for discontinuation symptoms on stopping, and limited efficacy with standard antidepressants, TMS is a game changer.
Considering a new treatment option can feel risky, and investing in the hope of recovery makes you vulnerable to more disappointment, especially for sufferers who are repeatedly resistant to medication. This quiz has been devised to help give you an indication of whether TMS could provide a remedy for you.
Is TMS Right For Me?
Take the short quiz below to see if you might be a good candidate for TMS.
It is important to stress that this quiz does not replace a full psychiatric evaluation and the questions cannot capture every individual circumstance. Still, it can confirm if TMS could be a viable treatment option and help with the decision to invest in a comprehensive consultation with a TMS Professional. The answers you give should be your honest reaction to the questions. On completion, you will be given an indication if TMS may be an option to consider and how best to move forward.
What is TMS Therapy and how does it work?
Transcranial Magnetic Stimulation, or TMS, may sound complicated so breaking each word down can remove some of the mystery.
Putting all this together, we see that during TMS a magnetic field is passed across the skull to stimulate neurons on the surface of the brain. The brain uses electrical connections to function. In depression these connections are often underactive, and in anxiety, they can be overactive. TMS introduces a non-invasive magnetic field to change electrical connectivity between neurons. By altering the field, TMS can correct over or under activity in the brain and relieve symptoms of depression and anxiety.
TMS therapy follows a schedule of daily treatments on weekdays over a 6-week period, followed by a taper over the last 3 weeks. These repetitive treatments change underlying electrical connections on the surface of the brain resulting in synaptic plasticity. Synaptic plasticity involves strengthening or correction of faulty neural pathways. Similar to an exercise routine or weight lifting, repeat treatments gradually build up stronger and healthier connections in the brain resulting in long lasting relief from depressive and anxiety symptoms.
Meeting the TMS Insurance Coverage Criteria
Take the short quiz below to see if you'll meet the TMS insurance coverage criteria.
During a course of TMS therapy, patients can drive themselves to and from sessions and can go about their day as usual following treatments. During the treatments, patients can watch tv, listen to music, meditate, or chat with their technician, whilst seated in a reclining chair. The TMS coil delivers magnetic pulses targeting the affected areas of the brain.
The beauty of TMS is that it is a non-invasive outpatient procedure and requires no anesthesia or medication of any type to deliver the treatment. It also does not cause any systemic side effects. The success rate for relief from depressive symptoms in our clinic is over 70%. We typically see similar results for many other conditions such as anxiety or PTSD.
Read more:
How does TMS therapy work? →
Who should avoid TMS Therapy?
Prior to any TMS treatment, your TMS doctor will take you through a series of questions about your medical history to ensure that
TMS is the right therapy for you. This will include identifying any contraindications to TMS:
Who qualifies for TMS Therapy?
There are 2 elements to this question:
TMS can be a fast and very effective treatment for a spectrum of mental health disorders. Ongoing research has also shown effectiveness for treating such conditions as Major Depression, Generalized Anxiety, PTSD, OCD, Bipolar Depression, and smoking cessation.
To date, however, the only indication that all major medical insurers cover treatment for (outside Medicaid) is Treatment Resistant Major Depression. This means clinical depression that has not responded to medications and counseling. The general requirements for coverage are: age 18 years and older, a diagnosis of
Major Depressive Disorder, having tried 1-4 medications without response or having experienced side effects to medications, and an attempted course of psychotherapy. TMS is not approved with any current psychotic symptoms, current alcohol or drug abuse, or a history of seizures. TMS should also not be used when specific medical devices or metallic objects are present above the neck. Some insurers also cover more recently FDA approved indications - OCD and smoking cessation - but this is more limited. Other conditions are not covered by insurance.
So called off-label treatments that are not covered through insurance include depression that is more mild to moderate in severity, anxiety, Bipolar depression, and PTSD. Additional studies have looked into treating other neuropsychiatric conditions as well such as chronic headache or migraine, and tinnitus. When clinically indicated with a good supporting evidence base, these conditions can be pursued via our self-pay sliding scale. In addition, we do not charge additional fees for treating additional conditions when utilizing insurance benefits to treat concurrent Major Depression.
Call or schedule a free phone consultation with our doctor to see if you may be a good candidate for TMS therapy →
How quickly does TMS work?
Studies show that some patients notice improvement in mood in as little as 2 weeks, but for others, TMS may take 4 to 6 weeks to significantly reduce symptoms. Sometimes, patients also report initial or additional benefit following the full 36 sessions of a standard course of TMS. When utilizing accelerated treatment courses outside insurance (as this is not covered by insurance to date), patients often begin to experience relief in as little as 2 to 3 days. And full remission of symptoms can be seen in as little as 1 week with accelerated protocols. Maintenance TMS sessions can also be beneficial in preventing relapse and maintaining relief from depression and other mental health symptoms.
Does TMS treat PTSD?
iTMS can effectively treat PTSD when standard medication or therapy fails. It can offer a real change for PTSD sufferers. Treatment for PTSD is similar to TMS treatment for depression, but typically involves a different protocol and/or target location. We have seen similar response and remission rates for PTSD sufferers in our clinic and very commonly treat this along with Major Depression concurrently.
Read more:
TMS therapy for PTSD →
How long do the effects of TMS last?
Most patients report relief from their symptoms for at least 4-6 months. Approximately two out of three patients will maintain response in 12 months following treatment, if utilizing medications, therapy, and/or TMS reintroduction when applicable.¹ Many patients maintain mental well-being in excess of 12 months and a significant number report complete recovery beyond this.
Additionally, if you respond well to your first round of TMS, retreatment typically works very well and often seems to provide a more robust response than the first treatment course. Close to 90% of those seeking repeat treatment will experience benefit again if the first treatment round was beneficial.
How much does TMS cost?
TMS costs will depend on your treatment and your insurance provider. For treatment of Major Depression, TMS therapy is covered by all major insurances outside Medicaid (if primary/sole coverage). At Inspire TMS Denver, we determine prior to treatment start, any remaining deductible, copays, or coinsurance that you may owe. If you are pursuing off-label treatments that are not covered by insurance, such as an accelerated protocol, PTSD, or anxiety treatment, we offer a sliding scale based upon your household income. And often, PTSD, anxiety, and other psychiatric conditions co-exist with Major Depression. When using insurance for depression treatment, we do not charge extra for any additional off-label treatment targeting other symptoms.
Read more:
TMS Pricing and Insurance Coverage →
Does insurance cover TMS therapy?
Yes, all major medical insurance companies outside Medicaid cover TMS therapy when other depression remedies have failed. Insurers differ in their requirements, but many are becoming more accepting of TMS treatment by reducing their requirements for prior authorization. Many only require one to two failed medication trials and a prior therapy course to approve TMS for depression treatment.
Read more:
TMS Insurance Coverage →
What does TMS feel like?
The magnetic pulses delivered through TMS therapy can be difficult to describe, but have been characterized by patients as several different sensations, such as hair tugging, tapping, a localized electrical sensation, or even like a small woodpecker. Though sensitivity varies, the sensation should not be overtly painful. Sensitivity or any scalp tenderness tends to lessen or resolve with repeat treatments. Slight adjustments to coil location and stimulation intensity can also help relieve any discomfort.
Patients may also experience eyebrow or jaw twitching during each brief stimulation set due to the magnetic pulses stimulating superficial nerves around the targeted area. The twitching only occurs during the brief pulses and stops as soon as the treatment stops. The twitching sensation is not painful and is usually only described as an “unusual feeling”.
It is important to note that the vast majority of patients suffer no significant side effects during or after their treatments.
Read more:
TMS treatment expectations →
Is TMS therapy safe?
TMS is non-invasive and involves no medications to administer treatment. The treatment uses magnetic waves to trigger electrical firing in the cortex of the brain only about two to three centimeters in area and depth. There is a very small risk for seizure, but not more than when utilizing typical psychiatric medications. The most recent data points to less than one seizure per 60,000 treatments.² TMS is a very safe procedure and very well tolerated by patients.
Does TMS treat depression?
Absolutely. We see over 70% of our patients experience significant relief from depressive symptoms. This is similar to rates seen in a large registry of over 14,000 treated patients.³ This is significantly higher than repeat trials of antidepressants after medications have failed. TMS was FDA approved in 2008 for the treatment of treatment resistant major depression due to this finding. There have been numerous randomized controlled and open label studies since showing that TMS is an effective treatment for depression.
Read more:
TMS therapy for depression →
Is TMS harmful to the brain?
No, since being approved by the FDA in 2008 for the treatment of major depression, there have been no studies indicating any short or long-term adverse effects to the brain with TMS treatment when performed with appropriate protocols. There can be limited local side effects at the outset of treatment such as mild headache or scalp discomfort, but these have not been shown to persist or occur more commonly after completion of treatment compared to sham (those not receiving TMS treatment). Likewise, no other adverse events have been identified as occurring more commonly compared to patients receiving sham treatment.
Can TMS make you worse?
Sometimes during treatment, patients may experience what is commonly referred to as a ‘dip.’ After a period of no real change or maybe after appreciating an initial improvement in mood, some patients infrequently describe a period where their mood decreases again. For some this dip in mood can be mild and short-lived, but for others it may be more intense and longer lasting. To date, we do not have a definitive scientific reason for why this dip sometimes occurs. The good news, however, is that we do see patients recover from the dip and respond to treatment.
One theory behind the dip is that when patients begin TMS treatment they often feel excited or hopeful about the potential for response from a novel treatment. This can result in a false sense of improvement, or an initial placebo response. As treatment moves along, this initial placebo response may dissipate, causing a ‘dip.’ Once treatment actually begins to work, however, (which can take several weeks) patients’ moods lift and they start to feel better again. While this seems like a logical explanation for ‘the dip,’ the ultimate reasoning for why this happens is still unknown.
It is important to communicate with providers about how you are feeling during any treatment course and to know that adjustments can be made to TMS treatment that may resolve problems with mood or anxiety. A different target location, adjustment to treatment intensity, or adding or removing off-label treatment may all be options. And if TMS ultimately is not successful, there are always additional treatment options available. Even for individuals that believe they have tried everything. If TMS treatment is not successful, your provider should recommend additional treatment options.
Read more:
TMS pros and cons →
Does TMS change your personality?
This is a yes and no question for good reason. TMS won’t alter anyone’s personality, but depression and anxiety disorders typically mask or negatively impact one’s true self. TMS can help free individuals from depressive and anxiety symptoms and allow people to be the best version of themselves.
Does TMS affect sleep?
Insomnia often occurs in the context of major depression, anxiety, PTSD, and other neuropsychiatric conditions. TMS has been shown to be effective in treating these conditions and so, not surprisingly, sleep disturbance also often improves with TMS treatment. Early on in treatment we have seen some patients experience mild insomnia, but this is rarely problematic. Sleep patterns often improve by the end of treatment.
Read more: TMS for sleep disorders →
What are the side effects of TMS?
Generally, TMS is very well tolerated with minimal or even no reported side effects. Those patients that do report side effects, usually describe mild headaches in the preliminary sessions. Some facial twitching can occur during sessions, caused by the stimulation indirectly affecting superficial nerves near the treatment site. But this is not painful. Scalp discomfort is also possible from the stimulation right beneath the coil, but typically is tolerable. Over the counter pain relievers can be utilized if necessary, but this is the minority of patients.
Is TMS the same as shock therapy? (ECT)
No, this can be a common misconception about TMS. ECT is typically utilized as a last resort and for serious episodes of mental collapse such as catatonia, debilitating depression with psychotic features, or treatment of refractory psychosis or mania. It requires sedation and a full medical team in an inpatient surgical setting as the purpose is to induce seizures to reset neural pathways. It is also essential to have a period of recovery in the hospital. TMS is a non-invasive procedure requiring no sedation or medications that is safely administered in an outpatient setting. Patients are wide awake during treatment and can drive to and from appointments on their own. Daily routines can be continued during a course of TMS treatment.
Read more:
TMS vs ECT →
Does TMS help bipolar?
There is some conflicting evidence on overall efficacy of TMS for Bipolar depression, but we have seen that TMS is clearly very effective for patients with this condition. Studies have shown similar response and remission rates for individuals with Bipolar depression.⁴ There may be a small risk for switching to mania with TMS, but recent reviews would suggest this is very rare and no more common than naturally occurs for this group of individuals.⁵ If utilized judiciously, the risk for manic switch should be very low. We have treated patients with Bipolar depression successfully at our clinic.
Read more:
TMS for bipolar disorder →
Does TMS treat anxiety?
Yes. TMS was cleared by the FDA for the treatment of Anxious Depression in 2021 for a specific coil on the Brainsway device. TMS is not approved, however, for treatment of Anxiety alone. Depression must still be present. There are very good studies showing that TMS works for treating anxiety and we have experienced similar results for treating anxiety compared to depression.⁶ There are different protocols to target anxiety relief.
Read more:
TMS for anxiety→
How long is TMS therapy?
The average treatment time in and out of the office is 15-30 minutes per day (depending on protocol utilized). Treatments take place five days per week each weekday, over six weeks. A taper is then utilized with three treatments week seven, two week eight, and finally one week nine. New TMS courses called
accelerated TMS can speed up the process into just five days of intensive treatment (10 sessions each day), but these are not covered yet by insurance. There was recent FDA approval for a specific accelerated protocol out of Stanford called SAINT/SNT. But it will take time before insurers may cover this protocol. Your TMS provider will discuss the different options and expected outcomes of treatment with you during your first consultation.
Can TMS impair memory?
The No, TMS should not impair memory. There is no evidence or indication of memory loss in 20+ years of treatment or research. Numerous studies point to quite the opposite, with many finding improvements in various domains related to overall cognitive performance, including memory.⁷ Conversely, Electroconvulsive treatment (ECT), sometimes confused with TMS, does often cause memory loss, especially surrounding the treatments.


Slide title
Write your caption hereButton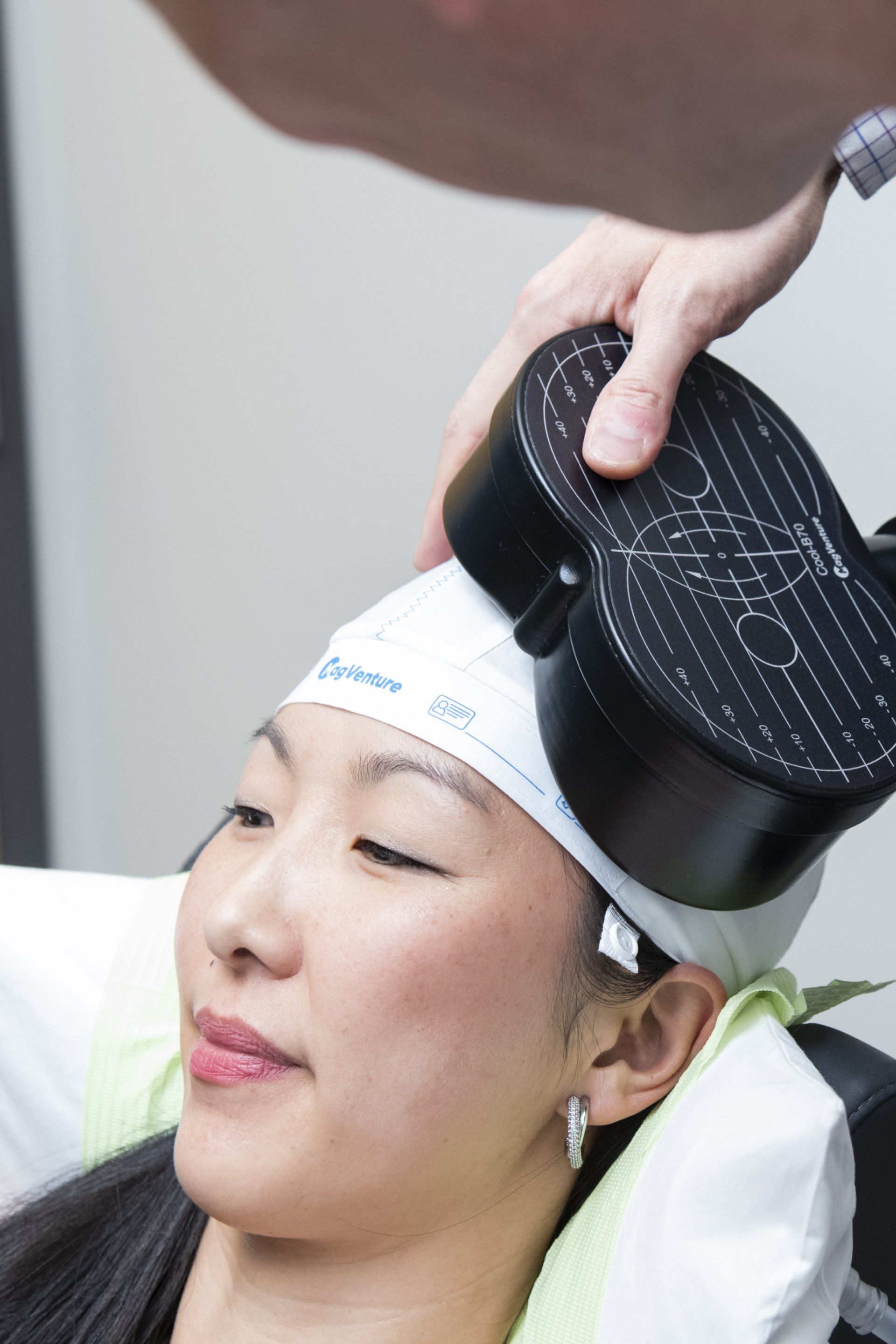
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
What Makes Us Different
Free TMS Therapy Guides, Quizzes & Phone Consultations


As Seen On Colorado's Best
For more visit our video library →
Awards & Accreditations
This is a paragraph. Writing in paragraphs lets visitors find what they are looking for quickly and easily.
This is a paragraph. Writing in paragraphs lets visitors find what they are looking for quickly and easily.
This is a paragraph. Writing in paragraphs lets visitors find what they are looking for quickly and easily.
This is a paragraph. Writing in paragraphs lets visitors find what they are looking for quickly and easily.
This is a paragraph. Writing in paragraphs lets visitors find what they are looking for quickly and easily.
Company Name
the tms journey
A Step By Step Process

Book your free telephone consultation with Dr. Clinch and use this time to ask any questions or voice any concerns about TMS. If there are no contraindications to treatment, you are a good candidate, and you wish to proceed with a full evaluation, we will schedule a full intake. You will be sent an invite to our confidential patient portal and forms for review and completion that expedite care.
Shortly after this, you will be seen in person for the full TMS evaluation. This will provide adequate information for us to then submit prior authorization for TMS coverage to your insurer. If seeking care off-label through self-pay, prior authorization is not needed. We then schedule your first and all subsequent treatment sessions. We obtain prior authorization and inform you of all costs prior to starting care.
Come in for your first treatment which starts with a 'mapping' to establish your unique treatment intensity and location. Following this and at all subsequent sessions, you will recline in a motorized chair, similar to a dental visit. You can then relax, listen to music, watch TV, read or chat during the treatment. At the end of your sessions, you can drive and return to your day as normal.
Samuel B. Clinch, M.D
Medical Director
Our shared inspiration is to alleviate mental illness and improve the mental wellbeing of the patients we treat. We respect all backgrounds and cultures and want to hear our patient’s stories to best guide care. During treatment, we reinforce positive wellness practices, help maximize lifestyle modifications, and integrate rTMS therapy into a patient’s overall mental and physical health treatment.


Patient Testimonials
Previous Patients Putting Your Mind At Rest

Amazing staff. They do a great job of explaining everything so definitely call if you’re still thinking about it. I had depression that kept me in bed for days. Since the middle of treatment I actually want to do things, and then I’m actually doing them. Completely recommend!
Communication throughout the process was absolutely excellent!! “Bedside manner” from all 3 was excellent. Office was excellent. Just cannot think of anything to critique about process from beginning to end, including pricing! Many thanks!!
Free Consultation
Call 720-446-8675 now, or complete the form below to request a call back.
Contact Us
We will get back to you as soon as possible.
Please try again later.
Contact Us
LOCATION
340 East 1st Avenue, Suite 333
Broomfield, CO 80020
What Happens After I Send My Message?
A member of our team will confirm your free consultation appointment within one business day.
Discover if TMS is right for you and answer all your queries about treatment, eligibility and costs.
Take the First Step Towards Your Mental Well-being Today
Transcranial Magnetic Stimulation (TMS) Therapy is an excellent treatment option for depression and anxiety with extensive research supporting its results, but how can you know if it is the right treatment for you?
We all experience low mood or overwhelming stress at times. However, these feelings can persist and develop into mental health conditions, such as Major Depressive Disorder, Generalized Anxiety Disorder, or Panic Disorder. These can be recurrent or potentially long-term conditions that impact your day-to-day life. Symptoms can present with no obvious cause or be in reaction to stressful events in our lives.
Frontline treatments for depression and anxiety usually consist of antidepressants and counseling. For many, this can be an effective solution for recovery and relief from depression and anxiety. Unfortunately, this does not work for everyone. Some ⅓ of all individuals seeking treatment will experience treatment resistant depression or fail to respond to standard treatments.¹
Transcranial Magnetic Stimulation (TMS) is an alternative option for patients who do not find relief with medication or therapy, or who suffer from adverse side effects from antidepressants.
To decide if TMS is right for you, we recommending asking yourself the following 4 questions:
-
1. Do I have a mental health condition that TMS is indicated for?
TMS is FDA-approved for treating major depressive disorder (MDD) and obsessive-compulsive disorder (OCD). It can also be used off-label to treat other mental health conditions such as anxiety, panic, and post-traumatic stress disorder (PTSD). If you have been diagnosed with any of these conditions, TMS could be a good treatment option for you.
-
2. Have I tried other treatment options?
Since insurance typically doesn't cover TMS unless you have tried other treatment options such as medication, therapy, or a combination of both, TMS is generally considered a second-line option. Although each insurer’s criteria varies, we generally recommend trying at least 2 different medications from different classes (eg an SSRI - Lexapro, Celexa, Zoloft, Prozac, Paxil; SNRI - Pristiq, Effexor, Cymbaltal; NDRI - Wellbutrin; or some other class of antidepressant - TCA, Lithium, Remeron, Abilify). We also recommend trying counseling.
-
3. Do I have any contraindications for TMS?
While TMS is generally safe and very well tolerated, some conditions may prevent you from receiving treatment or insurance may not cover treatment due to insufficient evidence base for your particular condition. These include a history of seizures, metal implants or magnetically influenced devices in your head, diagnosis of Schizophrenia or Bipolar, current psychotic symptoms, or current substance abuse. Please know that some of these conditions may still be suitable for treatment, but will need to be pursued via self-pay as insurance unfortunately does not cover TMS for these diagnoses.
-
4. Are you able to commit to TMS?
TMS therapy is a considerable time commitment, consisting of 36 total treatments that take place over 9 weeks. The first 6 weeks you receive 5 treatments a week, Monday through Friday. The last 3 weeks you are on a taper schedule with 3 treatments one week, 2 treatments the next week, and one treatment on your final week. Each appointment in the office typically lasts about 30 minutes.
TMS was originally approved by the FDA and later adopted by health insurance companies for treatment-resistant depression and our results with TMS speak for themselves,
https://www.inspiretmsdenver.com/inspire-tms-clinic-results
We achieve excellent results for depression, anxiety, PTSD, and OCD, offering a medication-free treatment option with only limited and localized minor side effects at most. Given the not uncommon side effects, potential for discontinuation symptoms on stopping, and limited efficacy with standard antidepressants, TMS is a game changer.
Considering a new treatment option can feel risky, and investing in the hope of recovery makes you vulnerable to more disappointment, especially for sufferers who are repeatedly resistant to medication. This quiz has been devised to help give you an indication of whether TMS could provide a remedy for you.
Is TMS Right For Me?
Take the short quiz below to see if you might be a good candidate for TMS.
It is important to stress that this quiz does not replace a full psychiatric evaluation and the questions cannot capture every individual circumstance. Still, it can confirm if TMS could be a viable treatment option and help with the decision to invest in a comprehensive consultation with a TMS Professional. The answers you give should be your honest reaction to the questions. On completion, you will be given an indication if TMS may be an option to consider and how best to move forward.
What is TMS Therapy and how does it work?
Transcranial Magnetic Stimulation, or TMS, may sound complicated so breaking each word down can remove some of the mystery.
Putting all this together, we see that during TMS a magnetic field is passed across the skull to stimulate neurons on the surface of the brain. The brain uses electrical connections to function. In depression these connections are often underactive, and in anxiety, they can be overactive. TMS introduces a non-invasive magnetic field to change electrical connectivity between neurons. By altering the field, TMS can correct over or under activity in the brain and relieve symptoms of depression and anxiety.
TMS therapy follows a schedule of daily treatments on weekdays over a 6-week period, followed by a taper over the last 3 weeks. These repetitive treatments change underlying electrical connections on the surface of the brain resulting in synaptic plasticity. Synaptic plasticity involves strengthening or correction of faulty neural pathways. Similar to an exercise routine or weight lifting, repeat treatments gradually build up stronger and healthier connections in the brain resulting in long lasting relief from depressive and anxiety symptoms.
During a course of TMS therapy, patients can drive themselves to and from sessions and can go about their day as usual following treatments. During the treatments, patients can watch tv, listen to music, meditate, or chat with their technician, whilst seated in a reclining chair. The TMS coil delivers magnetic pulses targeting the affected areas of the brain.
The beauty of TMS is that it is a non-invasive outpatient procedure and requires no anesthesia or medication of any type to deliver the treatment. It also does not cause any systemic side effects. The success rate for relief from depressive symptoms in our clinic is over 70%. We typically see similar results for many other conditions such as anxiety or PTSD.
Read more:
How does TMS therapy work? →
Who should avoid TMS Therapy?
Prior to any TMS treatment, your TMS doctor will take you through a series of questions about your medical history to ensure that
TMS is the right therapy for you. This will include identifying any contraindications to TMS:
Who qualifies for TMS Therapy?
There are 2 elements to this question:
TMS can be a fast and very effective treatment for a spectrum of mental health disorders. Ongoing research has also shown effectiveness for treating such conditions as Major Depression, Generalized Anxiety, PTSD, OCD, Bipolar Depression, and smoking cessation.
To date, however, the only indication that all major medical insurers cover treatment for (outside Medicaid) is Treatment Resistant Major Depression. This means clinical depression that has not responded to medications and counseling. The general requirements for coverage are: age 18 years and older, a diagnosis of
Major Depressive Disorder, having tried 1-4 medications without response or having experienced side effects to medications, and an attempted course of psychotherapy. TMS is not approved with any current psychotic symptoms, current alcohol or drug abuse, or a history of seizures. TMS should also not be used when specific medical devices or metallic objects are present above the neck. Some insurers also cover more recently FDA approved indications - OCD and smoking cessation - but this is more limited. Other conditions are not covered by insurance.
So called off-label treatments that are not covered through insurance include depression that is more mild to moderate in severity, anxiety, Bipolar depression, and PTSD. Additional studies have looked into treating other neuropsychiatric conditions as well such as chronic headache or migraine, and tinnitus. When clinically indicated with a good supporting evidence base, these conditions can be pursued via our self-pay sliding scale. In addition, we do not charge additional fees for treating additional conditions when utilizing insurance benefits to treat concurrent Major Depression.
Call or schedule a free phone consultation with our doctor to see if you may be a good candidate for TMS therapy →
How quickly does TMS work?
Studies show that some patients notice improvement in mood in as little as 2 weeks, but for others, TMS may take 4 to 6 weeks to significantly reduce symptoms. Sometimes, patients also report initial or additional benefit following the full 36 sessions of a standard course of TMS. When utilizing accelerated treatment courses outside insurance (as this is not covered by insurance to date), patients often begin to experience relief in as little as 2 to 3 days. And full remission of symptoms can be seen in as little as 1 week with accelerated protocols. Maintenance TMS sessions can also be beneficial in preventing relapse and maintaining relief from depression and other mental health symptoms.
Does TMS treat PTSD?
iTMS can effectively treat PTSD when standard medication or therapy fails. It can offer a real change for PTSD sufferers. Treatment for PTSD is similar to TMS treatment for depression, but typically involves a different protocol and/or target location. We have seen similar response and remission rates for PTSD sufferers in our clinic and very commonly treat this along with Major Depression concurrently.
Read more:
TMS therapy for PTSD →
How long do the effects of TMS last?
Most patients report relief from their symptoms for at least 4-6 months. Approximately two out of three patients will maintain response in 12 months following treatment, if utilizing medications, therapy, and/or TMS reintroduction when applicable.¹ Many patients maintain mental well-being in excess of 12 months and a significant number report complete recovery beyond this.
Additionally, if you respond well to your first round of TMS, retreatment typically works very well and often seems to provide a more robust response than the first treatment course. Close to 90% of those seeking repeat treatment will experience benefit again if the first treatment round was beneficial.
How much does TMS cost?
TMS costs will depend on your treatment and your insurance provider. For treatment of Major Depression, TMS therapy is covered by all major insurances outside Medicaid (if primary/sole coverage). At Inspire TMS Denver, we determine prior to treatment start, any remaining deductible, copays, or coinsurance that you may owe. If you are pursuing off-label treatments that are not covered by insurance, such as an accelerated protocol, PTSD, or anxiety treatment, we offer a sliding scale based upon your household income. And often, PTSD, anxiety, and other psychiatric conditions co-exist with Major Depression. When using insurance for depression treatment, we do not charge extra for any additional off-label treatment targeting other symptoms.
Read more:
TMS Pricing and Insurance Coverage →
Does insurance cover TMS therapy?
Yes, all major medical insurance companies outside Medicaid cover TMS therapy when other depression remedies have failed. Insurers differ in their requirements, but many are becoming more accepting of TMS treatment by reducing their requirements for prior authorization. Many only require one to two failed medication trials and a prior therapy course to approve TMS for depression treatment.
Read more:
TMS Insurance Coverage →
What does TMS feel like?
The magnetic pulses delivered through TMS therapy can be difficult to describe, but have been characterized by patients as several different sensations, such as hair tugging, tapping, a localized electrical sensation, or even like a small woodpecker. Though sensitivity varies, the sensation should not be overtly painful. Sensitivity or any scalp tenderness tends to lessen or resolve with repeat treatments. Slight adjustments to coil location and stimulation intensity can also help relieve any discomfort.
Patients may also experience eyebrow or jaw twitching during each brief stimulation set due to the magnetic pulses stimulating superficial nerves around the targeted area. The twitching only occurs during the brief pulses and stops as soon as the treatment stops. The twitching sensation is not painful and is usually only described as an “unusual feeling”.
It is important to note that the vast majority of patients suffer no significant side effects during or after their treatments.
Read more:
TMS treatment expectations →
Is TMS therapy safe?
TMS is non-invasive and involves no medications to administer treatment. The treatment uses magnetic waves to trigger electrical firing in the cortex of the brain only about two to three centimeters in area and depth. There is a very small risk for seizure, but not more than when utilizing typical psychiatric medications. The most recent data points to less than one seizure per 60,000 treatments.² TMS is a very safe procedure and very well tolerated by patients.
Does TMS treat depression?
Absolutely. We see over 70% of our patients experience significant relief from depressive symptoms. This is similar to rates seen in a large registry of over 14,000 treated patients.³ This is significantly higher than repeat trials of antidepressants after medications have failed. TMS was FDA approved in 2008 for the treatment of treatment resistant major depression due to this finding. There have been numerous randomized controlled and open label studies since showing that TMS is an effective treatment for depression.
Read more:
TMS therapy for depression →
Is TMS harmful to the brain?
No, since being approved by the FDA in 2008 for the treatment of major depression, there have been no studies indicating any short or long-term adverse effects to the brain with TMS treatment when performed with appropriate protocols. There can be limited local side effects at the outset of treatment such as mild headache or scalp discomfort, but these have not been shown to persist or occur more commonly after completion of treatment compared to sham (those not receiving TMS treatment). Likewise, no other adverse events have been identified as occurring more commonly compared to patients receiving sham treatment.
Can TMS make you worse?
Sometimes during treatment, patients may experience what is commonly referred to as a ‘dip.’ After a period of no real change or maybe after appreciating an initial improvement in mood, some patients infrequently describe a period where their mood decreases again. For some this dip in mood can be mild and short-lived, but for others it may be more intense and longer lasting. To date, we do not have a definitive scientific reason for why this dip sometimes occurs. The good news, however, is that we do see patients recover from the dip and respond to treatment.
One theory behind the dip is that when patients begin TMS treatment they often feel excited or hopeful about the potential for response from a novel treatment. This can result in a false sense of improvement, or an initial placebo response. As treatment moves along, this initial placebo response may dissipate, causing a ‘dip.’ Once treatment actually begins to work, however, (which can take several weeks) patients’ moods lift and they start to feel better again. While this seems like a logical explanation for ‘the dip,’ the ultimate reasoning for why this happens is still unknown.
It is important to communicate with providers about how you are feeling during any treatment course and to know that adjustments can be made to TMS treatment that may resolve problems with mood or anxiety. A different target location, adjustment to treatment intensity, or adding or removing off-label treatment may all be options. And if TMS ultimately is not successful, there are always additional treatment options available. Even for individuals that believe they have tried everything. If TMS treatment is not successful, your provider should recommend additional treatment options.
Read more:
TMS pros and cons →
Does TMS change your personality?
This is a yes and no question for good reason. TMS won’t alter anyone’s personality, but depression and anxiety disorders typically mask or negatively impact one’s true self. TMS can help free individuals from depressive and anxiety symptoms and allow people to be the best version of themselves.
Does TMS affect sleep?
Insomnia often occurs in the context of major depression, anxiety, PTSD, and other neuropsychiatric conditions. TMS has been shown to be effective in treating these conditions and so, not surprisingly, sleep disturbance also often improves with TMS treatment. Early on in treatment we have seen some patients experience mild insomnia, but this is rarely problematic. Sleep patterns often improve by the end of treatment.
Read more: TMS for sleep disorders →
What are the side effects of TMS?
Generally, TMS is very well tolerated with minimal or even no reported side effects. Those patients that do report side effects, usually describe mild headaches in the preliminary sessions. Some facial twitching can occur during sessions, caused by the stimulation indirectly affecting superficial nerves near the treatment site. But this is not painful. Scalp discomfort is also possible from the stimulation right beneath the coil, but typically is tolerable. Over the counter pain relievers can be utilized if necessary, but this is the minority of patients.
Is TMS the same as shock therapy? (ECT)
No, this can be a common misconception about TMS. ECT is typically utilized as a last resort and for serious episodes of mental collapse such as catatonia, debilitating depression with psychotic features, or treatment of refractory psychosis or mania. It requires sedation and a full medical team in an inpatient surgical setting as the purpose is to induce seizures to reset neural pathways. It is also essential to have a period of recovery in the hospital. TMS is a non-invasive procedure requiring no sedation or medications that is safely administered in an outpatient setting. Patients are wide awake during treatment and can drive to and from appointments on their own. Daily routines can be continued during a course of TMS treatment.
Read more:
TMS vs ECT →
Does TMS help bipolar?
There is some conflicting evidence on overall efficacy of TMS for Bipolar depression, but we have seen that TMS is clearly very effective for patients with this condition. Studies have shown similar response and remission rates for individuals with Bipolar depression.⁴ There may be a small risk for switching to mania with TMS, but recent reviews would suggest this is very rare and no more common than naturally occurs for this group of individuals.⁵ If utilized judiciously, the risk for manic switch should be very low. We have treated patients with Bipolar depression successfully at our clinic.
Read more:
TMS for bipolar disorder →
Does TMS treat anxiety?
Yes. TMS was cleared by the FDA for the treatment of Anxious Depression in 2021 for a specific coil on the Brainsway device. TMS is not approved, however, for treatment of Anxiety alone. Depression must still be present. There are very good studies showing that TMS works for treating anxiety and we have experienced similar results for treating anxiety compared to depression.⁶ There are different protocols to target anxiety relief.
Read more:
TMS for anxiety→
How long is TMS therapy?
The average treatment time in and out of the office is 15-30 minutes per day (depending on protocol utilized). Treatments take place five days per week each weekday, over six weeks. A taper is then utilized with three treatments week seven, two week eight, and finally one week nine. New TMS courses called
accelerated TMS can speed up the process into just five days of intensive treatment (10 sessions each day), but these are not covered yet by insurance. There was recent FDA approval for a specific accelerated protocol out of Stanford called SAINT/SNT. But it will take time before insurers may cover this protocol. Your TMS provider will discuss the different options and expected outcomes of treatment with you during your first consultation.
Can TMS impair memory?
The No, TMS should not impair memory. There is no evidence or indication of memory loss in 20+ years of treatment or research. Numerous studies point to quite the opposite, with many finding improvements in various domains related to overall cognitive performance, including memory.⁷ Conversely, Electroconvulsive treatment (ECT), sometimes confused with TMS, does often cause memory loss, especially surrounding the treatments.


Slide title
Write your caption hereButton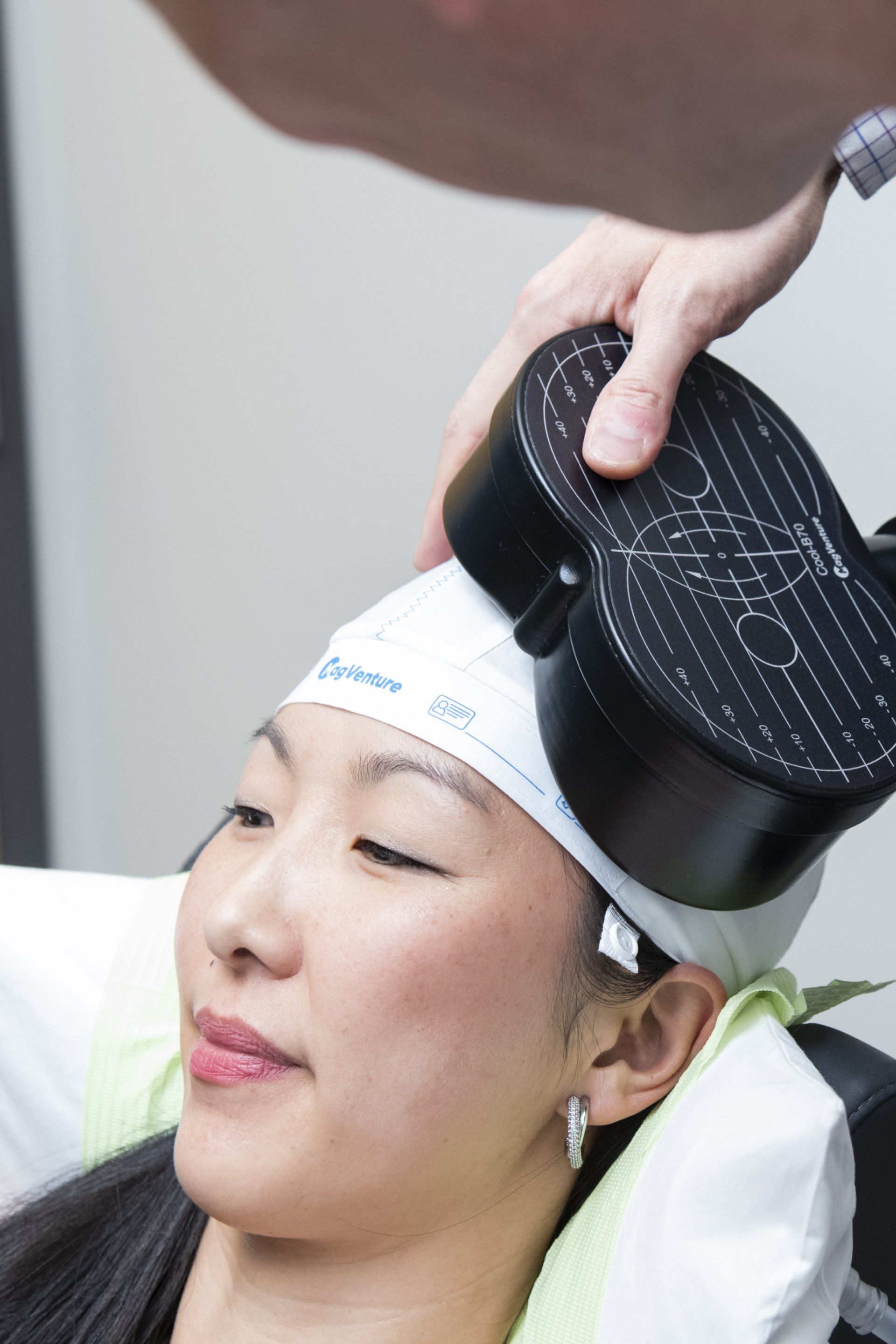
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
What Makes Us Different

Patient Testimonials
Previous Patients Putting Your Mind At Rest
I cannot say enough good things about Inspire TMS with the treatment, Dr. Clinch, and his staff. The treatment was very effective, helping me climb out of years of depression. Dr. Clinch is extremely knowledgeable, answered all my questions, and was very supportive, as was his staff.
Amazing staff. They do a great job of explaining everything so definitely call if you’re still thinking about it. I had depression that kept me in bed for days. Since the middle of treatment I actually want to do things, and then I’m actually doing them. Completely recommend!
Communication throughout the process was absolutely excellent!! “Bedside manner” from all 3 was excellent. Office was excellent. Just cannot think of anything to critique about process from beginning to end, including pricing! Many thanks!!
For more visit our Google reviews →
the tms journey
A Step By Step Process
Book your free telephone consultation with Dr. Clinch and use this time to ask any questions or voice any concerns about TMS. If there are no contraindications to treatment, you are a good candidate, and you wish to proceed with a full evaluation, we will schedule a full intake. You will be sent an invite to our confidential patient portal and forms for review and completion that expedite care.
Shortly after this, you will be seen in person for the full TMS evaluation. This will provide adequate information for us to then submit prior authorization for TMS coverage to your insurer. If seeking care off-label through self-pay, prior authorization is not needed. We then schedule your first and all subsequent treatment sessions. We obtain prior authorization and inform you of all costs prior to starting care.
Come in for your first treatment which starts with a 'mapping' to establish your unique treatment intensity and location. Following this and at all subsequent sessions, you will recline in a motorized chair, similar to a dental visit. You can then relax, listen to music, watch TV, read or chat during the treatment. At the end of your sessions, you can drive and return to your day as normal.
Our shared inspiration is to alleviate mental illness and improve the mental wellbeing of the patients we treat. We respect all backgrounds and cultures and want to hear our patient’s stories to best guide care. During treatment, we reinforce positive wellness practices, help maximize lifestyle modifications, and integrate rTMS therapy into a patient’s overall mental and physical health treatment.
Samuel B. Clinch, M.D
Medical Director
Free Consultation
Call 720-446-8675 now, or complete the form below to request a call back.
Contact Us
We will get back to you as soon as possible.
Please try again later.
Contact Us
LOCATION
340 East 1st Avenue, Suite 333
Broomfield, CO 80020
What Happens After I Send My Message?
A member of our team will confirm your free consultation appointment within one business day.
Discover if TMS is right for you and answer all your queries about treatment, eligibility and costs.
Take the First Step Towards Your Mental Well-being Today
Transcranial Magnetic Stimulation (TMS) Therapy is an excellent treatment option for depression and anxiety with extensive research supporting its results, but how can you know if it is the right treatment for you?
We all experience low mood or overwhelming stress at times. However, these feelings can persist and develop into mental health conditions, such as Major Depressive Disorder, Generalized Anxiety Disorder, or Panic Disorder. These can be recurrent or potentially long-term conditions that impact your day-to-day life. Symptoms can present with no obvious cause or be in reaction to stressful events in our lives.
Frontline treatments for depression and anxiety usually consist of antidepressants and counseling. For many, this can be an effective solution for recovery and relief from depression and anxiety. Unfortunately, this does not work for everyone. Some ⅓ of all individuals seeking treatment will experience treatment resistant depression or fail to respond to standard treatments.¹
Transcranial Magnetic Stimulation (TMS) is an alternative option for patients who do not find relief with medication or therapy, or who suffer from adverse side effects from antidepressants.
To decide if TMS is right for you, we recommending asking yourself the following 4 questions:
-
1. Do I have a mental health condition that TMS is indicated for?
TMS is FDA-approved for treating major depressive disorder (MDD) and obsessive-compulsive disorder (OCD). It can also be used off-label to treat other mental health conditions such as anxiety, panic, and post-traumatic stress disorder (PTSD). If you have been diagnosed with any of these conditions, TMS could be a good treatment option for you.
-
2. Have I tried other treatment options?
Since insurance typically doesn't cover TMS unless you have tried other treatment options such as medication, therapy, or a combination of both, TMS is generally considered a second-line option. Although each insurer’s criteria varies, we generally recommend trying at least 2 different medications from different classes (eg an SSRI - Lexapro, Celexa, Zoloft, Prozac, Paxil; SNRI - Pristiq, Effexor, Cymbaltal; NDRI - Wellbutrin; or some other class of antidepressant - TCA, Lithium, Remeron, Abilify). We also recommend trying counseling.
-
3. Do I have any contraindications for TMS?
While TMS is generally safe and very well tolerated, some conditions may prevent you from receiving treatment or insurance may not cover treatment due to insufficient evidence base for your particular condition. These include a history of seizures, metal implants or magnetically influenced devices in your head, diagnosis of Schizophrenia or Bipolar, current psychotic symptoms, or current substance abuse. Please know that some of these conditions may still be suitable for treatment, but will need to be pursued via self-pay as insurance unfortunately does not cover TMS for these diagnoses.
-
4. Are you able to commit to TMS?
TMS therapy is a considerable time commitment, consisting of 36 total treatments that take place over 9 weeks. The first 6 weeks you receive 5 treatments a week, Monday through Friday. The last 3 weeks you are on a taper schedule with 3 treatments one week, 2 treatments the next week, and one treatment on your final week. Each appointment in the office typically lasts about 30 minutes.
TMS was originally approved by the FDA and later adopted by health insurance companies for treatment-resistant depression and our results with TMS speak for themselves,
https://www.inspiretmsdenver.com/inspire-tms-clinic-results
We achieve excellent results for depression, anxiety, PTSD, and OCD, offering a medication-free treatment option with only limited and localized minor side effects at most. Given the not uncommon side effects, potential for discontinuation symptoms on stopping, and limited efficacy with standard antidepressants, TMS is a game changer.
Considering a new treatment option can feel risky, and investing in the hope of recovery makes you vulnerable to more disappointment, especially for sufferers who are repeatedly resistant to medication. This quiz has been devised to help give you an indication of whether TMS could provide a remedy for you.
Is TMS Right For Me?
Take the short quiz below to see if you might be a good candidate for TMS.
It is important to stress that this quiz does not replace a full psychiatric evaluation and the questions cannot capture every individual circumstance. Still, it can confirm if TMS could be a viable treatment option and help with the decision to invest in a comprehensive consultation with a TMS Professional. The answers you give should be your honest reaction to the questions. On completion, you will be given an indication if TMS may be an option to consider and how best to move forward.
What is TMS Therapy and how does it work?
Transcranial Magnetic Stimulation, or TMS, may sound complicated so breaking each word down can remove some of the mystery.
Putting all this together, we see that during TMS a magnetic field is passed across the skull to stimulate neurons on the surface of the brain. The brain uses electrical connections to function. In depression these connections are often underactive, and in anxiety, they can be overactive. TMS introduces a non-invasive magnetic field to change electrical connectivity between neurons. By altering the field, TMS can correct over or under activity in the brain and relieve symptoms of depression and anxiety.
TMS therapy follows a schedule of daily treatments on weekdays over a 6-week period, followed by a taper over the last 3 weeks. These repetitive treatments change underlying electrical connections on the surface of the brain resulting in synaptic plasticity. Synaptic plasticity involves strengthening or correction of faulty neural pathways. Similar to an exercise routine or weight lifting, repeat treatments gradually build up stronger and healthier connections in the brain resulting in long lasting relief from depressive and anxiety symptoms.
Meeting the TMS Insurance Coverage Criteria
Take the short quiz below to see if you'll meet the TMS insurance coverage criteria.
During a course of TMS therapy, patients can drive themselves to and from sessions and can go about their day as usual following treatments. During the treatments, patients can watch tv, listen to music, meditate, or chat with their technician, whilst seated in a reclining chair. The TMS coil delivers magnetic pulses targeting the affected areas of the brain.
The beauty of TMS is that it is a non-invasive outpatient procedure and requires no anesthesia or medication of any type to deliver the treatment. It also does not cause any systemic side effects. The success rate for relief from depressive symptoms in our clinic is over 70%. We typically see similar results for many other conditions such as anxiety or PTSD.
Read more:
How does TMS therapy work? →
Who should avoid TMS Therapy?
Prior to any TMS treatment, your TMS doctor will take you through a series of questions about your medical history to ensure that
TMS is the right therapy for you. This will include identifying any contraindications to TMS:
Who qualifies for TMS Therapy?
There are 2 elements to this question:
TMS can be a fast and very effective treatment for a spectrum of mental health disorders. Ongoing research has also shown effectiveness for treating such conditions as Major Depression, Generalized Anxiety, PTSD, OCD, Bipolar Depression, and smoking cessation.
To date, however, the only indication that all major medical insurers cover treatment for (outside Medicaid) is Treatment Resistant Major Depression. This means clinical depression that has not responded to medications and counseling. The general requirements for coverage are: age 18 years and older, a diagnosis of
Major Depressive Disorder, having tried 1-4 medications without response or having experienced side effects to medications, and an attempted course of psychotherapy. TMS is not approved with any current psychotic symptoms, current alcohol or drug abuse, or a history of seizures. TMS should also not be used when specific medical devices or metallic objects are present above the neck. Some insurers also cover more recently FDA approved indications - OCD and smoking cessation - but this is more limited. Other conditions are not covered by insurance.
So called off-label treatments that are not covered through insurance include depression that is more mild to moderate in severity, anxiety, Bipolar depression, and PTSD. Additional studies have looked into treating other neuropsychiatric conditions as well such as chronic headache or migraine, and tinnitus. When clinically indicated with a good supporting evidence base, these conditions can be pursued via our self-pay sliding scale. In addition, we do not charge additional fees for treating additional conditions when utilizing insurance benefits to treat concurrent Major Depression.
Call or schedule a free phone consultation with our doctor to see if you may be a good candidate for TMS therapy →
How quickly does TMS work?
Studies show that some patients notice improvement in mood in as little as 2 weeks, but for others, TMS may take 4 to 6 weeks to significantly reduce symptoms. Sometimes, patients also report initial or additional benefit following the full 36 sessions of a standard course of TMS. When utilizing accelerated treatment courses outside insurance (as this is not covered by insurance to date), patients often begin to experience relief in as little as 2 to 3 days. And full remission of symptoms can be seen in as little as 1 week with accelerated protocols. Maintenance TMS sessions can also be beneficial in preventing relapse and maintaining relief from depression and other mental health symptoms.
Does TMS treat PTSD?
iTMS can effectively treat PTSD when standard medication or therapy fails. It can offer a real change for PTSD sufferers. Treatment for PTSD is similar to TMS treatment for depression, but typically involves a different protocol and/or target location. We have seen similar response and remission rates for PTSD sufferers in our clinic and very commonly treat this along with Major Depression concurrently.
Read more:
TMS therapy for PTSD →
How long do the effects of TMS last?
Most patients report relief from their symptoms for at least 4-6 months. Approximately two out of three patients will maintain response in 12 months following treatment, if utilizing medications, therapy, and/or TMS reintroduction when applicable.¹ Many patients maintain mental well-being in excess of 12 months and a significant number report complete recovery beyond this.
Additionally, if you respond well to your first round of TMS, retreatment typically works very well and often seems to provide a more robust response than the first treatment course. Close to 90% of those seeking repeat treatment will experience benefit again if the first treatment round was beneficial.
How much does TMS cost?
TMS costs will depend on your treatment and your insurance provider. For treatment of Major Depression, TMS therapy is covered by all major insurances outside Medicaid (if primary/sole coverage). At Inspire TMS Denver, we determine prior to treatment start, any remaining deductible, copays, or coinsurance that you may owe. If you are pursuing off-label treatments that are not covered by insurance, such as an accelerated protocol, PTSD, or anxiety treatment, we offer a sliding scale based upon your household income. And often, PTSD, anxiety, and other psychiatric conditions co-exist with Major Depression. When using insurance for depression treatment, we do not charge extra for any additional off-label treatment targeting other symptoms.
Read more:
TMS Pricing and Insurance Coverage →
Does insurance cover TMS therapy?
Yes, all major medical insurance companies outside Medicaid cover TMS therapy when other depression remedies have failed. Insurers differ in their requirements, but many are becoming more accepting of TMS treatment by reducing their requirements for prior authorization. Many only require one to two failed medication trials and a prior therapy course to approve TMS for depression treatment.
Read more:
TMS Insurance Coverage →
What does TMS feel like?
The magnetic pulses delivered through TMS therapy can be difficult to describe, but have been characterized by patients as several different sensations, such as hair tugging, tapping, a localized electrical sensation, or even like a small woodpecker. Though sensitivity varies, the sensation should not be overtly painful. Sensitivity or any scalp tenderness tends to lessen or resolve with repeat treatments. Slight adjustments to coil location and stimulation intensity can also help relieve any discomfort.
Patients may also experience eyebrow or jaw twitching during each brief stimulation set due to the magnetic pulses stimulating superficial nerves around the targeted area. The twitching only occurs during the brief pulses and stops as soon as the treatment stops. The twitching sensation is not painful and is usually only described as an “unusual feeling”.
It is important to note that the vast majority of patients suffer no significant side effects during or after their treatments.
Read more:
TMS treatment expectations →
Is TMS therapy safe?
TMS is non-invasive and involves no medications to administer treatment. The treatment uses magnetic waves to trigger electrical firing in the cortex of the brain only about two to three centimeters in area and depth. There is a very small risk for seizure, but not more than when utilizing typical psychiatric medications. The most recent data points to less than one seizure per 60,000 treatments.² TMS is a very safe procedure and very well tolerated by patients.
Does TMS treat depression?
Absolutely. We see over 70% of our patients experience significant relief from depressive symptoms. This is similar to rates seen in a large registry of over 14,000 treated patients.³ This is significantly higher than repeat trials of antidepressants after medications have failed. TMS was FDA approved in 2008 for the treatment of treatment resistant major depression due to this finding. There have been numerous randomized controlled and open label studies since showing that TMS is an effective treatment for depression.
Read more:
TMS therapy for depression →
Is TMS harmful to the brain?
No, since being approved by the FDA in 2008 for the treatment of major depression, there have been no studies indicating any short or long-term adverse effects to the brain with TMS treatment when performed with appropriate protocols. There can be limited local side effects at the outset of treatment such as mild headache or scalp discomfort, but these have not been shown to persist or occur more commonly after completion of treatment compared to sham (those not receiving TMS treatment). Likewise, no other adverse events have been identified as occurring more commonly compared to patients receiving sham treatment.
Can TMS make you worse?
Sometimes during treatment, patients may experience what is commonly referred to as a ‘dip.’ After a period of no real change or maybe after appreciating an initial improvement in mood, some patients infrequently describe a period where their mood decreases again. For some this dip in mood can be mild and short-lived, but for others it may be more intense and longer lasting. To date, we do not have a definitive scientific reason for why this dip sometimes occurs. The good news, however, is that we do see patients recover from the dip and respond to treatment.
One theory behind the dip is that when patients begin TMS treatment they often feel excited or hopeful about the potential for response from a novel treatment. This can result in a false sense of improvement, or an initial placebo response. As treatment moves along, this initial placebo response may dissipate, causing a ‘dip.’ Once treatment actually begins to work, however, (which can take several weeks) patients’ moods lift and they start to feel better again. While this seems like a logical explanation for ‘the dip,’ the ultimate reasoning for why this happens is still unknown.
It is important to communicate with providers about how you are feeling during any treatment course and to know that adjustments can be made to TMS treatment that may resolve problems with mood or anxiety. A different target location, adjustment to treatment intensity, or adding or removing off-label treatment may all be options. And if TMS ultimately is not successful, there are always additional treatment options available. Even for individuals that believe they have tried everything. If TMS treatment is not successful, your provider should recommend additional treatment options.
Read more:
TMS pros and cons →
Does TMS change your personality?
This is a yes and no question for good reason. TMS won’t alter anyone’s personality, but depression and anxiety disorders typically mask or negatively impact one’s true self. TMS can help free individuals from depressive and anxiety symptoms and allow people to be the best version of themselves.
Does TMS affect sleep?
Insomnia often occurs in the context of major depression, anxiety, PTSD, and other neuropsychiatric conditions. TMS has been shown to be effective in treating these conditions and so, not surprisingly, sleep disturbance also often improves with TMS treatment. Early on in treatment we have seen some patients experience mild insomnia, but this is rarely problematic. Sleep patterns often improve by the end of treatment.
Read more: TMS for sleep disorders →
What are the side effects of TMS?
Generally, TMS is very well tolerated with minimal or even no reported side effects. Those patients that do report side effects, usually describe mild headaches in the preliminary sessions. Some facial twitching can occur during sessions, caused by the stimulation indirectly affecting superficial nerves near the treatment site. But this is not painful. Scalp discomfort is also possible from the stimulation right beneath the coil, but typically is tolerable. Over the counter pain relievers can be utilized if necessary, but this is the minority of patients.
Is TMS the same as shock therapy? (ECT)
No, this can be a common misconception about TMS. ECT is typically utilized as a last resort and for serious episodes of mental collapse such as catatonia, debilitating depression with psychotic features, or treatment of refractory psychosis or mania. It requires sedation and a full medical team in an inpatient surgical setting as the purpose is to induce seizures to reset neural pathways. It is also essential to have a period of recovery in the hospital. TMS is a non-invasive procedure requiring no sedation or medications that is safely administered in an outpatient setting. Patients are wide awake during treatment and can drive to and from appointments on their own. Daily routines can be continued during a course of TMS treatment.
Read more:
TMS vs ECT →
Does TMS help bipolar?
There is some conflicting evidence on overall efficacy of TMS for Bipolar depression, but we have seen that TMS is clearly very effective for patients with this condition. Studies have shown similar response and remission rates for individuals with Bipolar depression.⁴ There may be a small risk for switching to mania with TMS, but recent reviews would suggest this is very rare and no more common than naturally occurs for this group of individuals.⁵ If utilized judiciously, the risk for manic switch should be very low. We have treated patients with Bipolar depression successfully at our clinic.
Read more:
TMS for bipolar disorder →
Does TMS treat anxiety?
Yes. TMS was cleared by the FDA for the treatment of Anxious Depression in 2021 for a specific coil on the Brainsway device. TMS is not approved, however, for treatment of Anxiety alone. Depression must still be present. There are very good studies showing that TMS works for treating anxiety and we have experienced similar results for treating anxiety compared to depression.⁶ There are different protocols to target anxiety relief.
Read more:
TMS for anxiety→
How long is TMS therapy?
The average treatment time in and out of the office is 15-30 minutes per day (depending on protocol utilized). Treatments take place five days per week each weekday, over six weeks. A taper is then utilized with three treatments week seven, two week eight, and finally one week nine. New TMS courses called
accelerated TMS can speed up the process into just five days of intensive treatment (10 sessions each day), but these are not covered yet by insurance. There was recent FDA approval for a specific accelerated protocol out of Stanford called SAINT/SNT. But it will take time before insurers may cover this protocol. Your TMS provider will discuss the different options and expected outcomes of treatment with you during your first consultation.
Can TMS impair memory?
The No, TMS should not impair memory. There is no evidence or indication of memory loss in 20+ years of treatment or research. Numerous studies point to quite the opposite, with many finding improvements in various domains related to overall cognitive performance, including memory.⁷ Conversely, Electroconvulsive treatment (ECT), sometimes confused with TMS, does often cause memory loss, especially surrounding the treatments.


Slide title
Write your caption hereButton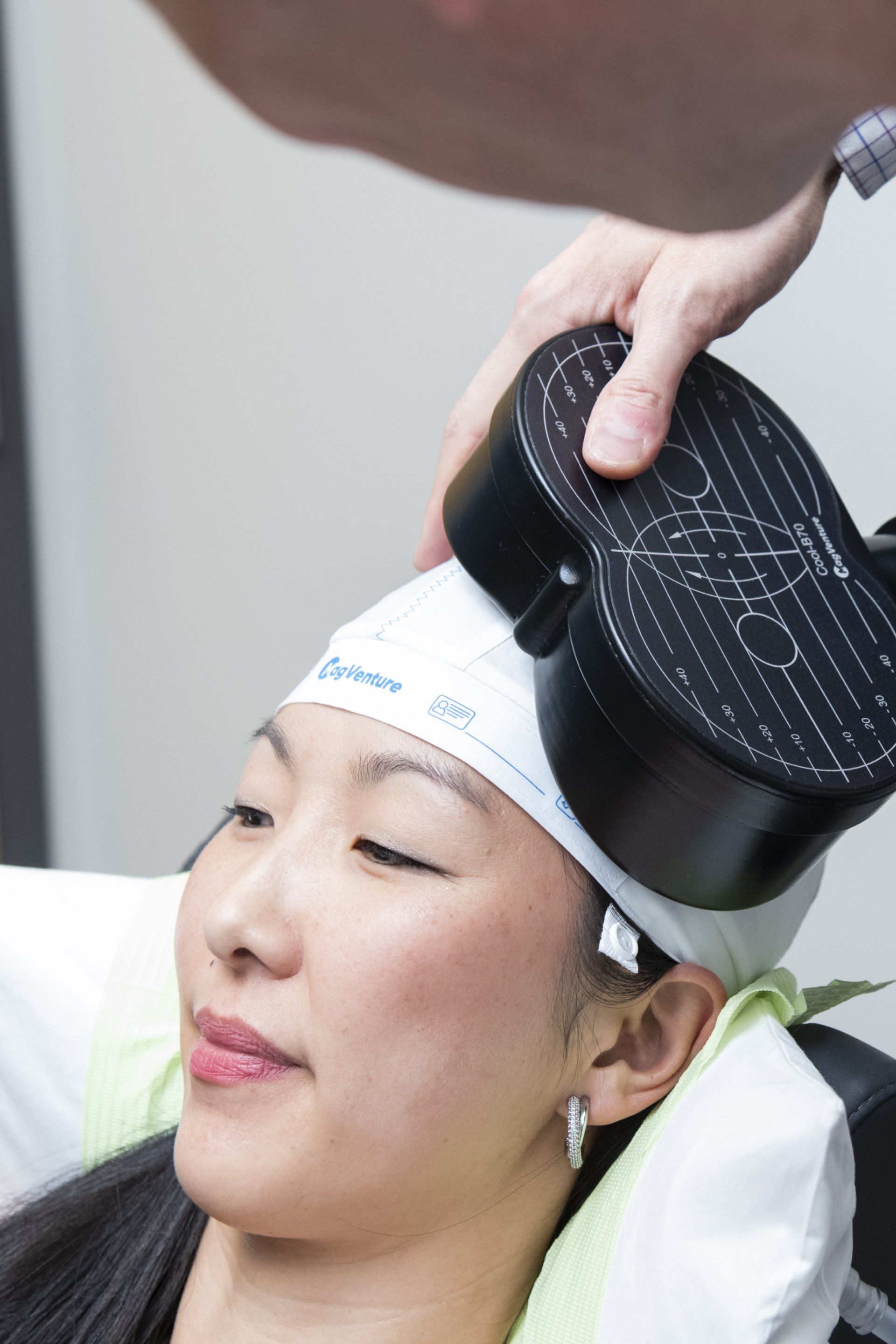
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
What Makes Us Different

Patient Testimonials
Previous Patients Putting Your Mind At Rest
I cannot say enough good things about Inspire TMS with the treatment, Dr. Clinch, and his staff. The treatment was very effective, helping me climb out of years of depression. Dr. Clinch is extremely knowledgeable, answered all my questions, and was very supportive, as was his staff.
Amazing staff. They do a great job of explaining everything so definitely call if you’re still thinking about it. I had depression that kept me in bed for days. Since the middle of treatment I actually want to do things, and then I’m actually doing them. Completely recommend!
Communication throughout the process was absolutely excellent!! “Bedside manner” from all 3 was excellent. Office was excellent. Just cannot think of anything to critique about process from beginning to end, including pricing! Many thanks!!
For more visit our Google reviews →
the tms journey
A Step By Step Process
Book your free telephone consultation with Dr. Clinch and use this time to ask any questions or voice any concerns about TMS. If there are no contraindications to treatment, you are a good candidate, and you wish to proceed with a full evaluation, we will schedule a full intake. You will be sent an invite to our confidential patient portal and forms for review and completion that expedite care.
Shortly after this, you will be seen in person for the full TMS evaluation. This will provide adequate information for us to then submit prior authorization for TMS coverage to your insurer. If seeking care off-label through self-pay, prior authorization is not needed. We then schedule your first and all subsequent treatment sessions. We obtain prior authorization and inform you of all costs prior to starting care.
Come in for your first treatment which starts with a 'mapping' to establish your unique treatment intensity and location. Following this and at all subsequent sessions, you will recline in a motorized chair, similar to a dental visit. You can then relax, listen to music, watch TV, read or chat during the treatment. At the end of your sessions, you can drive and return to your day as normal.
Our shared inspiration is to alleviate mental illness and improve the mental wellbeing of the patients we treat. We respect all backgrounds and cultures and want to hear our patient’s stories to best guide care. During treatment, we reinforce positive wellness practices, help maximize lifestyle modifications, and integrate rTMS therapy into a patient’s overall mental and physical health treatment.
Samuel B. Clinch, M.D
Medical Director
Free Consultation
Call 720-446-8675 now, or complete the form below to request a call back.
Contact Us
We will get back to you as soon as possible.
Please try again later.
Contact Us
MAIN OFFICE
720-446-8675
LOCATION
340 East 1st Avenue, Suite 333
Broomfield, CO 80020
What Happens After I Send My Message?
A member of our team will confirm your free consultation appointment within one business day.
Discover if TMS is right for you and answer all your queries about treatment, eligibility and costs.
Take the First Step Towards Your Mental Wellbeing Today
Our Services
Learning Hub
Quick Links
Our Services
Learning Hub
Quick Links
Committed
to Your Individual
Care & Recovery
Our Services
Learning Hub
Quick Links
Business Hours
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
Find Us
LOCATION
PHONE & FAX
720-446-8675 | 720-798-6969
All Rights Reserved | Inspire TMS Denver
Information on this site is for reference purposes only. It is not intended to be nor should it be taken as medical advice. Individuals should see a medical professional regarding their symptoms.
Website by Leo Cook Digital Marketing
Committed
to Your Individual
Care & Recovery
Business Hours
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
Find Us
LOCATION
PHONE
720-446-8675 | 720-798-6969
Information on this site is for reference purposes only. It is not intended to be nor should it be taken as medical advice. Individuals should see a medical professional regarding their symptoms.
All Rights Reserved | Inspire TMS Denver
Website by Leo Cook Marketing
Business Hours
- Monday
- -
- Tuesday
- -
- Wednesday
- -
- Thursday
- -
- Friday
- -
- Saturday
- Closed
- Sunday
- Closed
Find Us
LOCATION
PHONE & FAX
720-446-8675 | 720-798-6969
National Suicide Prevention Lifeline


Emergencies Call 911
Receive help 24 hours a day
Information on this site is for reference purposes only. It is not intended to be nor should it be taken as medical advice. Individuals should see a medical professional regarding their symptoms.
All Rights Reserved | Inspire TMS Denver
Website by Leo Cook Digital Marketing