What are the Different Types of Depression?


Major Depressive Disorder (MDD) is a common mental health condition characterized by relentless feelings of sadness, loss of interest in activities, and low energy. However, this condition can present in various ways from person to person. There are 6 subtypes of clinical depression: melancholic, anxious, atypical, psychotic, seasonal, and postpartum depression. While there are distinct types of depression, each share common core symptoms. A detailed psychiatric evaluation is needed in order to diagnose any potential depressive subtypes. This additional exploration may help individuals better understand their depression and achieve better treatment outcomes. Read on to learn more about the features, challenges, and risk factors of the 6 subtypes of depression.
Melancholic Depression
25-30% of the depressed population is affected by melancholic depression, a type of depression categorized by severe feelings of emptiness, despair, and guilt that are unreactive to circumstances. Distinguishing features include a worsening of symptoms in the morning, inability to feel pleasure, weight loss, and insomnia from waking too early.
Learn more about
TMS treatment for depression →
Furthermore, individuals with melancholic depression rarely respond to psychotherapy or social interventions, suggesting a strong biological component. Hypercortisol has also been found to be associated with melancholia. Individuals with this depressive subtype are at a higher risk for unemployment.

Anxious Depression
Anxious depression is distinct from other subtypes because it includes symptoms of anxious distress. In addition to low mood and/or loss of interest in daily activities, individuals with anxious depression experience at least two of the following symptoms: restlessness, difficulty concentrating due to excessive worry, fear that something terrible might happen, feeling tense, or feeling that they might lose control of themselves. Although this depressive subtype can appear similar to comorbid anxiety and depression, it is distinct because individuals with anxious depression don’t actually meet the diagnostic criteria for an anxiety disorder.
Learn more about
TMS for anxiety →
It is estimated that
54-78% of individuals with depression also experience anxious distress. This distress is significant, and individuals with anxious depression experience more functional impairment with relationships, work, home life, and social situations. Women and individuals with a history of trauma or abuse are more likely to have anxious depression than non-anxious depression.

Atypical Depression
20-30% of depressed patients exhibit
atypical depression, a type of depression characterized by the ability to temporarily feel better in response to positive external events (mood reactivity), severe fatigue, hypersomnia, and increased appetite. Additionally, atypical depression appears to have an earlier age of onset and a chronic, long-lasting presentation. A key feature of atypical depression is rejection sensitivity where the patient frequently has an excessive response to rejection, leading to social impairment. Although it is not part of the diagnostic criteria, symptoms of atypical depression tend to worsen at night. Atypical depression may present more often in bipolar disorder, especially bipolar disorder type II. Two-thirds of the cases of atypical depression can also report symptoms of bipolarity.

Psychotic Depression
Psychotic depression is a subtype of major depression that includes primary symptoms of psychosis, hallucinations and/or delusions. Hallucinations are false sensory perceptions such as seeing or hearing things that aren’t real. Delusions are false, fixed beliefs. The delusions and hallucinations are almost always related to the individual’s depressed mood. For example, a patient might hear voices criticizing them, or telling them that they’re to blame for something. It is estimated that
10-15% of the depressed population also exhibit psychosis. Depressed individuals over the age of 60 are more likely to have psychotic depression. Furthermore, patients with psychotic depression are at a much higher risk for
suicide than non-psychotic depression. Individuals with active psychosis are out of touch with reality and often feel as if they are not in control of their life. Psychosis results in difficulties deciphering what is real and what is imagined, making everyday activities extremely challenging.

Seasonal Depression
An estimated
0.5-2.4% of the general population and 10-20% of those diagnosed with major depression are affected by
seasonal depression (also known as seasonal affective disorder or SAD), a subtype of depression that features season-specific depression. 90% of those with seasonal depression experience a winter-pattern with symptoms present in the winter months and absent in the spring and summer. Specific symptoms include hypersomnia, increased appetite, and social withdrawal. The remaining 10% exhibit a summer-pattern where symptoms including insomnia and decreased appetite appear in the summer months and subside in the fall and winter. Although the causes of seasonal affective disorder are complex, circadian rhythm disruption due to shifted night-day cycle contributes to the development of the disorder.

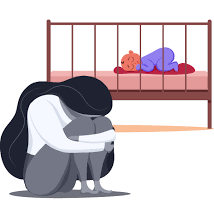
Postpartum Depression
Postpartum depression is a type of major depression that specifically appears during pregnancy or within the first four weeks following delivery. Relentless feelings of sadness, emptiness, and low mood affect the individual’s ability to function and adjust to their new baby. Although the research is less prevalent, postpartum depression can also affect fathers. First-time mothers and fathers have a higher risk of postpartum depression. The drastic change in hormones during and after pregnancy are implicated in postpartum depression. Although it is less common, postpartum depression can sometimes include psychotic features.
Read more onTMS for Postpartum Depression →
While all types of major depression share many primary features, understanding what makes your depression unique can help you better understand your specific needs and potentially improve treatment outcomes with treatment more targeted to your depression subtype. A detailed assessment is necessary in order to properly identify any depressive specifiers. TMS Therapy can be an effective treatment for all subtypes of depression. Contact us to learn if TMS is right for you!

Every Question Answered
Want to know more about TMS? Check out this in-depth guide to TMS therapy with transparent and easy to understand explanations about TMS processes, protocols, and treated conditions.
Latest Posts

















